Umoja Biopharma's Potential for First In Vivo CAR T To Enter Clinic

By Erin Harris, Editor-In-Chief, Cell & Gene
Follow Me On Twitter @ErinHarris_1
Last year, Seattle-based Umoja Biopharma’s CEO, Dr. Andy Scharenberg, joined me on Cell & Gene: The Podcast to discuss the evolution of allogeneic in vivo CAR T cell therapeutics. We also discussed The Climb, or The Colorado Laboratory and Innovation Manufacturing Building, the company's lentiviral vector development and manufacturing facility. The episode, which is well worth your time, was packed with valuable information about what’s to come for in vivo CAR T. Shortly thereafter, I invited Umoja's Co-Founder and CTO, Ryan Crisman, to be an expert panelist on Cell & Gene Live, Optimizing Your Cold Chain For Cell Therapies, to talk through practical ways to improve shipping systems, tracking, product monitoring, and more for both just-in-time delivery and cryogenic preservation. Clearly, the company is making large strides for in vivo CAR T cell therapies. So, when I heard the announcement about FDA clearance of its IND application for UB-VV111, a CD19 directed in situ CAR T for hematologic malignancies, I reached right out to Umoja for more information. I talked to Scharenberg and Chief Operating Officer, David Fontana, about Umoja’s expectations to initiate a Phase 1 study and to dose the first patient by the end of 2024, with the potential for UB-VV111 to become the first in vivo CAR T cell therapy to enter the clinic in the U.S. Here’s what they had to say.
Overall, what are the current limitations of ex vivo cellular immunotherapies?

What are the main safety concerns associated with in vivo CAR-T therapies? How does Umoja work to avoid them?
David Fontana: We are beginning the process now to collect clinical safety and efficacy data for our in vivo approach. Through our pre-clinical studies, we have not noticed any new toxicities tied to the in vivo approach—in fact, efficacy and safety signals in those models appear to potentially be even superior to the ex vivo CAR Ts being used today. Ultimately the proof will be in the clinic, and we are excited to initiate our U.S.-based Phase 1 clinical trial, named INVICTA-1, this year after clearance of our IND application from the FDA last week.
What are the main challenges in translating in vivo CAR T from preclinical models to clinical settings?

Talk to us about UB-VV111, VivoVec gene delivery platform, and their connection.
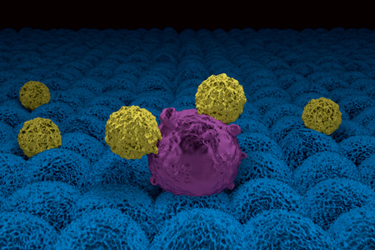
Andrew Scharenberg: VivoVec is our in vivo gene therapy delivery platform, a lentiviral particle system that allows us to turn any CAR or any binder into an in vivo-delivered and in situ-generated CAR T cell product. UB-VV111 is our first clinical-stage therapy from our VivoVec program, generating CD19 CAR T cells directly in a patient’s body, without the requirement for lymphodepleting chemotherapy used by both ex vivo autologous and allogeneic CAR T approaches today, nor the burdensome logistics that prevent the significant majority of patients from being treated with CAR Ts.
What’s on the horizon for in vivo CAR T?
David Fontana: 2024 is a pivotal year for the field of in vivo CAR T cell companies. As companies like ours initiate U.S. clinical trials, we hope that the promising patient outcomes afforded by CAR T cell therapies will become significantly more accessible and far reaching than what they are today. The ex vivo process is rate-limiting at most steps—especially in manufacturing as the industry continues to face challenges of viral vector shortages and slow ramp-ups of manufacturing capacity. We have built this company from Day 1 to eliminate these sorts of barriers, most especially when we decided to own our manufacturing in-house—a rare step for a pre-clinical biotech.
