Immunitas Therapeutics On The Future Of Immuno-Oncology

By Erin Harris, Editor-In-Chief, Cell & Gene
Follow Me On Twitter @ErinHarris_1
Immunitas Therapeutics, a single cell genomics-based drug discovery company, recently announced the publication of Inhibitory CD161 Receptor Identified in Gliomas-infiltrating T cells by Single Cell Analysis in the journal, Cell. I talked to Kai Wucherpfenning, M.D., Ph.D., corresponding author, Professor and Chair of the Department of Cancer Immunology and Virology at the Dana-Farber Cancer Institute, Professor of Neurology at Harvard Medical School, and scientific co-founder of Immunitas Therapeutics about the role robotic automation plays in immunology, the use of single-cell RNA sequencing in the study, as well as the future of immun0-oncology.
Briefly explain Immunitas Therapeutics.
Wucherpfenning: Immunitas is an immuno-oncology therapeutics company advancing multiple programs to the clinic. Immunitas’ programs are derived from a cross-functional, highly integrated, single cell genomics platform that enables rapid target identification and validation in parallel with antibody discovery and engineering. IMT-009, a first-in-class T & NK cell modulator targeting CD161, is being developed for the treatment of solid tumors and hematological malignancies. The company was founded by the Longwood Fund with leading scientists from Dana Farber, MGH, the Broad, and MIT. In 2019, Immunitas raised a $39M Series A from a strong syndicate of investors also including Hillhouse, NVF, Leaps by Bayer, and M Ventures.
What role does robotic automation play in immunology overall? And why is robotic automation changing the immunology landscape?
 Wucherpfenning: Robotic automation is an important tool in most modern biology labs. The ability to replicate processes at small scale across multiple samples allows us to really expand our data sets and therefore our understanding of underlying biological activity. For example, in the case of single cell sequencing, while pulling out one cell to sequence the RNA is something that can be done relatively easily by hand, to do this across thousands or even millions of cells is a place where automation is critically important. A big part of the power of single cell sequencing is the wealth of data that can be generated from relatively small numbers of tissue samples, because the data are multiplied by the number of cells in the sample, thanks in part to automation.
Wucherpfenning: Robotic automation is an important tool in most modern biology labs. The ability to replicate processes at small scale across multiple samples allows us to really expand our data sets and therefore our understanding of underlying biological activity. For example, in the case of single cell sequencing, while pulling out one cell to sequence the RNA is something that can be done relatively easily by hand, to do this across thousands or even millions of cells is a place where automation is critically important. A big part of the power of single cell sequencing is the wealth of data that can be generated from relatively small numbers of tissue samples, because the data are multiplied by the number of cells in the sample, thanks in part to automation.
Explain next generation sequencing in detail and how it is used to advance immunology.
Wucherpfenning: Single cell analysis and next generation sequencing are integral to understanding immune cell programs at high resolution. Next generation sequencing allows rapid sequencing of cDNA from large numbers of tumor cells and infiltrating immune cells. Computational techniques allow us to interpret these data and discover novel therapeutic targets. Single cell sequencing takes each cell within a given sample and sequences the RNA from each of those cells – generating detailed molecular information on gene expression for each of thousands or tens of thousands of cells. This gives researchers a rich data set to interrogate disease pathways even with small clinical samples.
Explain Immunitas’ platforms and how they shape target antibody interactions that drive immune diseases.
Wucherpfenning: Immunitas leverages a single cell sequencing platform (as was described in the paper) to identify and rapidly validate new targets for immuno-oncology using clinical samples. The platform thus enables discovery of the critical immune pathways directly in humans rather than attempting to ‘translate’ mouse data to humans. The platform can also be used to help guide biomarker and indication selection for clinical candidates. Further, Immunitas has built capabilities around antibody discovery and optimization that allows rapid pharmacological validation of targets as well as accelerates the pace to developing drugs that can be used in the clinical setting to help patients in need.
Immuno-oncology has relied for too long on a limited number of mouse models whose direct relevance to human cancer is unclear. Our single cell technology allows us to understand genetic circuits in human immune cells directly from the affected tissue.
What are the benefits of using immunotherapy to treat cancer?
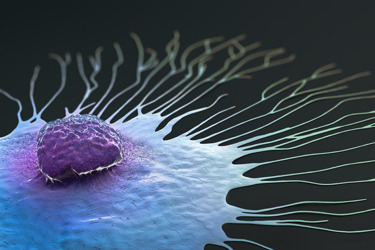
Wucherpfenning: Immunotherapy helps the patient’s own immune system to fight cancer. This is, in many ways, the first line of defense against cancer in healthy individuals, and what immunotherapy does is to help the existing defense mechanisms be more effective by targeting the key pathways by which tumors block an effective immune response.
Why did you use single-cell RNA sequencing for your study?
Wucherpfenning: With bulk RNA sequencing, it remains unclear in which cell types particular sets of genes are expressed. This issue greatly limits the use of bulk RNA-seq data to discover novel targets because tumors are extremely complex. Furthermore, in cancers most of the RNA originates from the tumor cells. Identifying key genes in immune cells within tumors is greatly advanced by use of a single cell approach.
How did you use single-cell RNA sequencing to reveal the new immunotherapy targets?
Wucherpfenning: We focused our analysis of tumor-infiltrating T cells because these are the cells responsible for clinical responses to immunotherapy. When T cells recognize a tumor antigen, they proliferate and clonally expand. We examined which genes are overexpressed in those T cells that respond to the tumor by clonal expansion. This analysis led to the discovery of the KLRB1 gene which encodes an inhibitory receptor in T cells.
What did your analysis reveal? What are these new targets?
Wucherpfenning: KLRB1, which encodes for the protein CD161, was one of the top scoring genes in the analysis. This inhibitory receptor had previously been described in NK cells (another type of immune cell), and when it engages with its ligand, which is found on tumor cells, the interaction suppresses the efficacy of both T and NK cells in killing of tumor cells. This was demonstrated through a series of experiments, including in vitro and in vivo work where KLRB1 was knocked out, and the function of the immune cells was increased.
Can you explain how these targets could be utilized in the fight against cancer?
Wucherpfenning: Because CD161 inhibits T and NK cell activation, an antibody that binds to this cell surface receptor can enhance their anti-tumor function in multiple common cancer types.
Could your process be used to identify more targets for immuno-oncology? How so?
Wucherpfenning: Absolutely. In fact, Immunitas Therapeutics was founded on that principle exactly — using these findings to create a drug targeting CD161 as well as using this technique to find other targets that can be used in the fight against cancer. The key to leveraging this technique is to have good data sets from human tumors and a focused biological question. Immunitas is working to expand their pipeline of programs by leveraging this approach.
Where is the field of immuno-oncology headed in the future?
Wucherpfenning: The field has been encouraged by the success of the PD1/PDL1 inhibitors. A tremendous amount of research is going on around this and a few other targets. We believe that new tools and techniques, like the ones used in this paper, will allow for more diverse targets being validated and drugged to help patients in need going forward.
We are very excited about these data and about the publication. Immunitas is driving programs towards the clinic based on this work, and we look forward to seeing this result in new treatments for patients.
