Gamma-Delta T-Cell Therapy for AML

By Erin Harris, Editor-In-Chief, Cell & Gene
Follow Me On Twitter @ErinHarris_1
IN8bio is a clinical-stage biopharma that’s developing cancer therapies using genetically modified gamma-delta T-cells to advance candidates for both liquid and solid tumors. William Ho, CEO at IN8bio, brought me up to speed on the company’s progress with gamma-delta T-cell-based immunotherapies and why they represent a groundbreaking approach in oncology, including treatment for Acute Myeloid Leukemia (AML).
Briefly describe IN8bio.

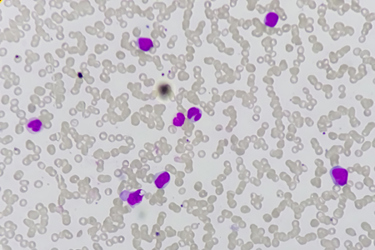
The innate and adaptive immune responses play critical roles in the fight against cancer. While both systems possess important functions, the most effective tumor killing occurs when they work together. Gamma-delta T cells are a unique subset of immune cells that sit at the nexus of the innate and adaptive systems and possess properties of both.
The science is based on the scalable manufacturing of these unique cells following decades of research by co-founder Lawrence Lamb and colleagues at the University of Alabama at Birmingham. Our mission is CANCER ZERO—the complete eradication of cancer cells in every patient.
How does the efficacy of gamma-delta T-cell therapy compare to other cellular immunotherapies such as CAR T-cells?
Gamma-delta T-cell therapy offers a promising alternative to conventional cellular immunotherapies like CAR T therapy. Unlike CAR T-cells, which are engineered to target specific antigens, gamma-delta T-cells possess innate immune capabilities that allow them to recognize and attack a broader range of cancer cells without prior modification. This flexibility reduces the likelihood of tumor escape and can lead to more durable responses.
First-generation CAR T-cells target CD19, which is expressed on both healthy and cancerous B cells, but for solid tumors and other leukemias, we need to preserve the healthy cells while attacking the tumor.
These unique cells also possess both innate and adaptive immune properties. They can respond rapidly to infections and tumors like innate immune cells while also providing antigen-specific responses akin to adaptive immune cells.
Their multifunctional nature and complex receptor repertoire allow these therapies to distinguish between healthy and cancerous cells. They can effectively kill tumor cells directly as well as recruit and activate additional immune effector cells to target and eradicate the tumor. Notably, gamma-delta T-cells can eliminate cancer cells without prior antigen priming and have the ability to antigen present and trigger a broader immune cell response. These properties make gamma-delta T-cells promising candidates for use in both solid and hematological cancer therapies.
Gamma-delta T-cell therapies represent a groundbreaking approach in oncology, with the potential to deliver broad and durable anti-tumor effects through a unique mechanism of action that complements and enhances existing treatments. This innovation offers new hope for patients, particularly those with cancers that have limited therapeutic options.
Regarding AML specifically, what are the unique features of gamma-delta T-cells that render them promising for cancer immunotherapy?
For Acute Myeloid Leukemia (AML), gamma-delta T-cells offer several unique advantages. They exhibit potent cytotoxic activity against cancer cells, even in the presence of immune-suppressive conditions typical of these malignancies. Gamma-delta T cells can recognize and destroy cancer cells through both antigen-dependent and antigen-independent mechanisms, enhancing their ability to target diverse and heterogeneous tumor cells. Additionally, they secrete pro-inflammatory cytokines that help recruit other immune cells to the tumor site, amplifying the anti-tumor response.
INB-100 is an allogeneic product candidate initially developed for the treatment of patients with acute leukemia undergoing hematopoietic bone marrow transplantation (HSCT). Our scientific founder, Dr. Lawrence Lamb, Ph.D., was the first to describe a survival benefit in HSCT patients with naturally elevated levels of gamma-delta T cells. INB-100 was designed to translate this observation into a treatment and provides donor derived allogeneic gamma-delta T cells to patients following their HSCT.
Updated positive clinical data has been reported from the Phase 1 investigator-sponsored trials of INB-100 for hematological malignancies. It has also been reported that IN8bio has completed a Type B meeting with the FDA and received guidance on the registrational path to advance INB-100 for the treatment of AML. Briefly bring us up to speed on INB-100 and share what’s next for this program.
We're currently focused on expanding our INB-100 trial to enroll additional patients—up to 10 more in this cohort. We're also planning to introduce a control group of AML patients to directly compare those receiving our gamma-delta immunotherapy with those receiving only standard-of-care treatment. We aim to complete enrollment for the INB-100 drug arm by the end of 2024, with long-term follow-up results expected in 2025.
Earlier this summer, we had a productive Type B meeting with the FDA, where we received guidance on advancing INB-100 as a post-transplant maintenance therapy for AML, with relapse-free survival as the primary endpoint.
We believe the outcomes in our INB-100 trial are already exceeding those of similar patients, including those with AML undergoing haploidentical transplantation with reduced intensity conditioning who aren't receiving INB-100.
