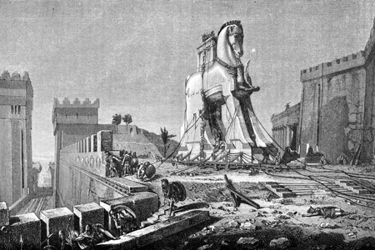
Using Stem Cells As An Immunologic 'Trojan Horse'

By Tyler Menichiello, Chief Editor, Bioprocess Online
Achieving effective, targeted delivery remains a longstanding challenge in the cell and gene therapy space. Whether delivering healthy copies of a gene to diseased tissues or directing cell therapies to tumor sites, successful treatment involves some level of evasion from the immune system — especially in cancer immunotherapy. Because while the body’s immune response is the very thing being leveraged by immunotherapies, it can also hinder the delivery of therapeutic agents — neutralizing them before they get to the target.
To overcome this immunogenicity challenge, Calidi Biotherapeutics is developing a unique, multimodal approach to cancer immunotherapy — one that combines oncolytic viruses with stem cells. Calidi’s two main programs, NeuroNova and SuperNova, utilize allogeneic stem cells as a “Trojan horse” to protect and deliver oncolytic viruses to the site of solid tumors, where they trigger a cancer-fighting immune response. SuperNova is the company’s newest program that uses adipose-derived mesenchymal stem cells (AD-MSC) to do this, and it’s set to begin Phase 1 trials later this year. To learn more about Calidi’s unique “Trojan horse” approach, I met with its CSO, Dr. Antonio Santidrian, Ph.D.
A Cellular Delivery Vector
“Many companies have tried different oncolytic viruses or viral vectors as biotherapeutics to treat cancer, but they haven’t seen major success in the clinic,” Santidrian tells me. He says this is likely due to premature viral clearance by the immune system. This viral elimination marks one of the biggest challenges facing these therapies — finding a balance between the anti-tumoral and anti-viral responses of the immune system. “Calidi realized the need to protect these viruses from the immune system,” he explains, “and we found the way to make that happen was to use stem cells.”
Loading oncolytic viruses into stem cells for delivery doesn’t just offer protection from the immune system — it also potentiates the virus and improves therapeutic potency. “The virus is able to amplify inside the stem cells, so the amount of virus we’re delivering to the tumor is much higher,” he explains.
Calidi’s NeuroNova (which has completed Phase 1 trials) combines neural stem cells with an oncolytic adenovirus for patients with glioblastoma. SuperNova, on the other hand, combines AD-MSCs with an oncolytic vaccinia virus to treat patients with solid tumors. Regarding the decision to use AD-MSCs, Santidrian says, “the scalability of these cells is much higher compared to other stem cells.”
One reason why, he says, is the abundant availability of raw starting material. “We can get more stem cells from fat or liposuctions, which gives us a bigger volume to start with.” The other reason for using AD-MSCs is their compatibility with the vaccinia virus.
Why Calidi Chose The Vaccinia Virus
Oncolytic viruses, by nature, infect tumor cells preferentially. Santidrian says there are three major mechanisms behind their efficacy. The first is the viruses’ ability to infect tumor cells and replicate inside them, eventually leading to the lysis of tumor cells. The second is the subsequent viral infection of surrounding endothelial cells — i.e., in blood vessels — which “collapses the vascularity” around the tumor. The third, “and potentially the most important,” he says, is the activation of the immune system.
In the company’s SuperNova candidate, the oncolytic virus of choice is the vaccinia virus. “We chose to use vaccinia virus because it is one of the more lytic and powerful viruses among the three (vaccinia, herpes, and adenovirus), and because vaccinia is not a human pathogen,” Santidrian explains. This makes it both a safe and effective virus to load into AD-MSCs. Vaccinia virus also contains double-stranded DNA, which according to Santidrian allows for the possibility of regional genetic modifications. “In the future, we can add any payload we want in the virus,” he says.
One of the key characteristics of vaccinia, and another reason the company chose it, is because of its ability to infect many tumor types. “Vaccinia virus is potentially the only virus that’s able to infect every tumor type,” Santidrian explains, “making it truly tumor agnostic.” This is compared to herpes and adenoviruses, which he says usually require certain receptors not found on all tumor types.
Investing In Development
In preparing SuperNova for the clinic, Sanditrian says NeuroNova was a major reference from a regulatory standpoint. “Phase 1 was completed on that program, so the concept of using stem cells to deliver a virus is already in the clinic,” he says. However, the clinical experience of NeuroNova didn’t make the process development for SuperNova any easier. “It’s complex to manufacture a virus, to manufacture cells, and then to actually manufacture a final product that is a combination of these two biologics,” he says. His advice to other biotechs in similar positions is to invest in in-house processes and analytical development. “This allows for a quick turnover of ideas and interaction with the discovery, translational, and technical operations teams. That is actually what makes a big difference in the company.”
As for what’s in store in 2024, Santidrian says Calidi is moving forward with the Phase 1 trial for SuperNova, while continuing research on NeuroNova. When asked about any potential challenges, he says, “I really don’t like to use the word ‘challenge,’ because there are established milestones you have to achieve, not challenges.”
“I don’t envision any challenges in our technology,” he continues, “we just have to follow the process and proceed with those clinical trials. We have the right talent, the right people, KOLs, and advisory board helping us on this path."
