Our Annual Cancer Immunotherapy Update
By Wayne Koberstein, Executive Editor, Life Science Leader
Follow Me On Twitter @WayneKoberstein
This article originally appeared in Life Science Leader magazine.
When we started our series, “Combination Cancer Immunotherapy — A Virtual Roundtable,” in 2014, our basic assumptions were not the consensus view. We assumed immunotherapy, now more commonly called immuno-oncology (IO), would become the dominant form of cancer treatment and central target of academic and industry research in oncology. We assumed a single, backbone therapy would become the pillar around which combinations of therapeutics with complementary targets would form. And we assumed the IO field, especially in its combination approaches, would pose profound scientific and business challenges as it took over as the central focus of oncology in general. Our assumptions turned out to be correct. Now, all IO has to do is catch up with itself.
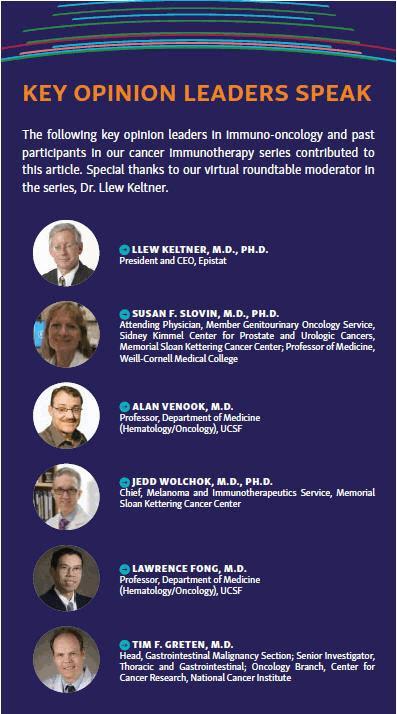 This annual update of our original series takes a look at recent research and commercial efforts to deal with the ramifications of the IO revolution. We have published two other IO Updates, in 2015 and 2016. This year, we spoke with some of the key opinion leaders who participated in the previous discussions, caught many of the key findings presented at the annual AACR conference in April, and looked at the topics likely to arise at the annual ASCO conference in June. Two major themes at both events will surely echo our first assumptions: First, immuno-oncology has climbed to the top of oncology more quickly than even its initial supporters imagined. Second, IO combinations will win adoption in practice based on continuing research into immune mechanisms alongside a massive effort in clinical development.
This annual update of our original series takes a look at recent research and commercial efforts to deal with the ramifications of the IO revolution. We have published two other IO Updates, in 2015 and 2016. This year, we spoke with some of the key opinion leaders who participated in the previous discussions, caught many of the key findings presented at the annual AACR conference in April, and looked at the topics likely to arise at the annual ASCO conference in June. Two major themes at both events will surely echo our first assumptions: First, immuno-oncology has climbed to the top of oncology more quickly than even its initial supporters imagined. Second, IO combinations will win adoption in practice based on continuing research into immune mechanisms alongside a massive effort in clinical development.
That research has gained momentum for more than “academic” reasons. The new immunotherapeutics, especially the PD-1 inhibitors such as Opdivo (nivolumab) and Keytruda (pembrolizumab), have shown they can produce lasting benefits for patients beyond anything seen before, but of course not for all patients all the time. As evident at AACR — and predictably so at ASCO and other related meetings — the IO community’s attention has largely shifted to the question of why cancers in some people respond to immunotherapy, why others do not respond or relapse later, and what can be done to turn non- or poor responders into good responders. Mechanistic understanding may be the main avenue toward new agents that outperform or boost the performance of the current ones. At the same time, however, leading researchers and companies have taken the empirical route with hundreds of clinical trials probing new possibilities.
One answer to the responder/nonresponder issue is that the picture seems to improve as new trial data comes out and approvals for new drugs and indications mount up. One of our regular KOL contributors, Jedd Wolchok, M.D., Ph.D., of Memorial Sloan Kettering Cancer Center (MSK), sees the promising data arising from continuing development of the first two approved drugs in the class. Wolchok and his team have been conducting some of the seminal trials with checkpoint inhibitors, as well as other immune-modifying agents as potential complements.
“The combination of CTLA-4 and PD-1 blockade in melanoma with ipilimumab and nivolumab was approved late in 2015, but we got the first glimpse at the survival data from the Phase 3 study at AACR this year, with the very fortunate outcome that the number of patients who died on the study was well below projections based upon prior data. Thus, there is still no median OS reached for the PD-1 blockade or the combination blockade group,” Wolchok says. “Of course, it is good to see how much progress has been made in melanoma, but it is great to see the same combination in later-stage trials across different disease types using doses and schedules that have been adapted to maximize safety in each type. We have a lot of work going on to optimize the use of the combination strategy in a large variety of solid tumors and hematologic malignancies.”
Susan Slovin, M.D., Ph.D., of MSK, agrees that immuno- oncology has progressed and, like most research leaders in this field, has an individual take on where it is headed: “There has been greater emphasis made on trying to understand the tumor microenvironment and how the checkpoint inhibitors may influence specific immune populations. The new idea of tissue residual memory cells to provide immune surveillance is a novel concept under evaluation. Another important milestone is the impact of CAR [chimeric antigen receptor] T cells on the hematologic malignancies and several new approaches for their use in solid tumors.”
Alan Venook, M.D., of UCSF, who voiced the most skepticism about the new immunotherapies in our original virtual roundtable, has moderated his views since then, based on subsequent clinical data. “The biggest change has been the expansion of the population of patients and diseases who benefit from checkpoint inhibition,” he says. “Less dramatic, but still important, has been the evidence that combination inhibitors, such as CTLA-4 plus PD-1, are even more impactful. Obviously, these developments change the flavor of current and future research plans. I remain pessimistic of how broadly these will work and what long-term consequences might be, but both the breadth of activity across a number of diseases and, more importantly, the extraordinary responses we see in some otherwise refractory patients, make it clear that checkpoint inhibition has ushered in an entirely new era of immunotherapy.”
“Unfortunately, despite promising preclinical data, many novel immune therapies do not prove perfect within clinical trials,” says Slovin. “So we may be revolutionary in the moment for some diseases, but we still haven’t figured out why some cancers have minimal responses to the current armamentarium. That, to me, remains the most interesting question.”
QUICK STUDY
Day by day, our bodies fight cancer. Tiny spots of precancerous or cancerous cells rise up, only to die under the close scrutiny and powerful assault of the immune system. Occasionally, and in some individuals, part of the cancer survives and evolves by randomly adaptive mutation to protect itself from killer T cells and other immune cells that would ordinarily recognize and destroy it. The growing tumor avoids immune detection and response not by hiding behind a mask, but by performing a sort of cellular hypnosis, effectively turning the attacking cells off or even enlisting them as cancer co-conspirators.
Also called leukocytes or lymphocytes, T cells are classified by the CD (cluster of differentiation) number, such as CD8+, each one coded to a certain set of antigens the CD cell type expresses on its surface. T cells change identity and function by expressing different antigens. The same T cell can be a memory, killer, regulatory, or any other type, depending on the antigens it expresses. “Successful” tumors check an immune attack by evolving and adapting the ability to manipulate T cell identity, inactivating or turning memory (CD4+, CD8+, or TM) and killer (CD8+ or TK) T cells into regulatory (CD4+, CD25+, or Tregs) T cells that suppress immune response. Note: T cells that perform widely different functions can share the same CD codes; the antigenic variations between TM, TK, Tregs, and their various subsets, for example, are subtle and still far from completely understood — and therein lies one potential vein for extracting knowledge about the variable effectiveness of IO agents.
Checkpoints are essentially antigens that tumors induce T cells to express, typically turning the T cells into Tregs that shield the cancer from immune response. But the most significant defensive tool the tumor wields, PD-1 (programmed cell death protein 1), acts only partly as a checkpoint inhibitor, inactivating the CD8+ cells by binding them to the PD-L1 ligand on the tumor cell. PD-1 inhibitors also appear to up-regulate a host of TNF (tumor necrosis factor) receptors that stimulate populations of activated killer T cells to expand and attack the tumor.
So far, the clinical data supports the strategy of blocking PD-1 as superior to blocking its ligand, PD-L1. Also, research studies suggest the more a patient’s tumor expresses PD-1/PD-L1, the more likely the patient will respond positively to anti-PD-1 or anti-PD-L1 therapy. Still, the jury is out and having a big argument over that supposition, based on the questionable accuracy of biopsies assessing PD-L1 status in tumors, which are notoriously heterogeneous.
Yet the clinical results outweigh all kibitzing; anti- PD-1 works much, much better than older approaches — for so many more patients, with much more lasting benefit, and incomparable safety. Anti-PD-1 also significantly outperforms its closest IO competitor, anti-CTLA-4 (Yervoy/ipilimumab). Although less than 50 percent of treated patients may have a significant benefit, the positive results of anti-PD-1 are often dramatic and some believe they deserve the label “cure.”
Although the resounding theme at AACR projected a consensus about the anti-PD-1 predominance and we heard no one challenge its position directly, many presenters and some of the key opinion leaders we interviewed spoke of checkpoint inhibitors more equivalently. They usually mentioned anti-CTLA-4 in the same breath and are perhaps still looking for a new challenger to emerge from among the many other checkpoint candidates. Nevertheless, for the time being, the predominance of anti-PD-1 therapy in IO seems beyond question.
BIG KID ON THE BLOCK
Two large pharma companies, Merck (MSD outside the United States), and Bristol-Myers Squibb, now have a virtual monopoly on approved and candidate anti- PD-1 agents. Partners Merck KGaA and Pfizer are present in the space, as is AstraZeneca with its R&D arm MedImmune, and Roche/Genentech — all with their anti-PD-L1 drugs, though all lag behind. But the question of why most patients fail to respond to this backbone IO therapy has taken center stage in oncology research and kept the concept of therapeutic combinations alive.
These days, even if an oncology drug in development has no claim to being a stand-alone immunotherapy, the developer will likely attempt to position the asset as having potential complementary effects in an IO combination. And most often, the target combination will include anti-PD-1. No wonder, then, that the IO space seems preoccupied at the present with this question: What agent or agents will rise to the top as the best complements to anti-PD-1?
For the answer, though, you might have to watch only one company — Merck. Since Merck won the first FDA approval for its anti-PD-1 drug Keytruda (pembrolizumab) in 2014, it has thrown itself headlong into the IO field, buying up assets and launching an ever-lengthening list of clinical trials — most not paid for by Merck — to test the drug in a wide variety of combinations. No other IO-focused company matches Merck in the extent of partnerships and trials.
Why? Roy Baynes, head of global clinical development and chief medical officer at Merck Research Laboratories, has described how his team is building a “data wall” with the multitude of Keytruda combination trials. The trials reflect another trend in the industry’s IO development — they steadily expand the products’ target indications into almost every cancer type. Merck appears to believe, by January 1, 2018, it will have amassed so much data on Keytruda alone and in combinations, no other company will ever be able to climb over the wall to compete with its anti-PD-1 position.
“Baynes is absolutely correct,” says Dr. Llew Keltner, president and CEO of Epistat, who moderated our original virtual roundtable. “Merck has already won the early and mid-game because it is doing so many more combination trials than anyone else. It is doing the combination trials not because it’s trying to find out what companies to buy — it’s doing the trials because it wants to see what works. Treatments that work and can get approved in combination with Keytruda will increase Keytruda sales.”
People at AACR may well have been distracted from Merck’s onslaught by the buzz over IDO inhibitors, a class that has been one of the star candidates for improving response rates in checkpoint blockade. IDO (indoleamine-2,3-dioxygenase) is a “rate-limiting” enzyme in the tryptophan (TRP) to kynurenine (KYN) metabolic pathway, which keeps a lid on immunity.
This year, inhibiting IDO became the new great white hope in IO, and researchers presented multiple preclinical models at AACR supporting the concept. A Phase 2 trial by NewLink Genetics of its tryptophan metabolic pathway drug, indoximod, in combination with Keytruda, even generated some disappointment when its interim results showed “only” a 52 percent overall response rate (ORR) — 6 points lower than the ORR in Phase 1 results by a combo of Keytruda with Incyte’s anti-IDO drug, epacadostat. Incyte echoes Merck’s strategy of multiple partnerships and trials to amass data on its IO candidates in a variety of combinations. It has partnered with both Merck and BMS to conduct trials of their products in combos with epacadostat.
Among the Big Pharma IDO contenders, Pfizer is playing catchup in the class, in a deal with iTeos now at the Phase 1 stage in brain cancer. But Pfizer is also catching up in IO generally. After spending more than $3 billion for avelumab (Bavencio), an anti-PD-L1 drug and candidate for urogenital cancer, the company — with codeveloper Merck KGaA (EMD Serono) — won an FDA approval for the product in March 2107, but only in the rare indication of Merkel cell carcinoma. AstraZeneca/ MedImmune have an extended IO development program, but only one approval so far, for NSCLC candidate Imfinzi (durvalumab), in treating locally advanced or metastatic urothelial carcinoma (mUC). And Roche’s anti-PD-L1 atezolizumab (Tecentriq) recently failed unexpectedly in a Phase 3 urogenital cancer trial, adding fuel to the fire of speculation — long overdue — about the potential differences in mechanism of action and clinical response between different molecules in the anti-PD-1/PD-L1 class.
ANGLES OF PROGRESS
As clinical trials sort out the immunotherapy combinations empirically, two normally separate sectors, academia and industry, have joined the basic and preclinical research hunt for mechanistic understanding. The clinical progress of the past year has ironically revealed the lack of commensurate progress in probing the many factors that influence immunity at the level of cells, molecules, and the tumor microenvironment — one big avenue of hope for improving clinical response rates. Enumerating the relevant biomarkers alone is not enough; the pathways and junctions in the system interact, like the parts and pieces of a living reactor, to create the complex tug o’ war between immune activation and regulation.
The immune system is a metabolic system, where communication is usually not binary but comes in information-rich packages such as proteins. Academic and company scientists are working — sometimes separately, often together — to see the dynamic interaction inside immunity at a higher and higher resolution. The driving force behind the intense investigation and collaboration at the mechanistic level is the strong belief the efforts will lead to answers about how different patients respond to treatment and what treatments could make all patients respond better.
It would be a mistake, however, to see up-regulation of one immune component or cell type as always “good” and down-regulation of another component or cell type as always “bad.” An immune system activated by checkpoint blockade will express immuno-inhibiting components to regulate immune response. Under the spell of a tumor, Tregs may help defeat immune response, but working as part of an effective response, Tregs keep immunity from raging out of control and attacking healthy tissue. Right now, perhaps thousands of studies in academic and industrial settings are creatively resolving this moving micro-universe of immunity at a finer and finer grain. Clinical results are driving this quest for a more refined theory and structure as a basis for predicting which new therapeutic approaches might improve the results.
“Some of the cases of resistance to checkpoint blockade are ones where the innate wiring mechanisms of the immune system are actually being mutated or altered, which is a bit worrisome,” says Lawrence Fong, M.D., of UCSF. An original member of our virtual roundtable, Fong and his associates are leading clinical researchers in IO. “The mutations show the ability of the tumors to evade the immune response. That means we really need to think about multimodality therapies, including other therapeutic approaches that may not be dependent on that wiring of the immune system. There are not only ways to target the cancer cells through conventional means, but also other immunotherapeutic means that are not dependent on that signaling mechanism.”
One of our KOLs believes the most powerful lens for the job is genomics. “There is a lot of research into how and why IO works in some patients but does not work in others, which is very promising,” says Tim Greten, M.D., of the National Cancer Institute. Greten has been a participant in this series from the beginning and continues to conduct groundbreaking IO research at the NIH. “We are finally giving more and more attention to the correlation of genomics and immunotherapy — understanding the biology and how genes may affect immune responses, and how we can potentially combine genomics and immuno-oncology to prescribe the best therapies or therapeutic combinations for each patient. What I would like to see in oncology is for geneticists to get together with immuno-oncologists.”
“It’s extremely important to continue our research, because we need to understand mechanisms of action and we need to understand the pharmacodynamic effects of these combinations,” says Wolchok. “We need to know how the combinations are hitting their intended targets and then focus those particular combinations on particular subsets of patients who have a need for that specific combinatorial approach. We are really striving to understand how to make immunotherapy combinations a more precise intervention. There is a whole other world of trials combining checkpoint blockade with other forms of anticancer therapy, whether they be targeted therapies, chemotherapy, radiation therapy, or other means of local tumor destruction.”
Here stands the state of progress in combination cancer immunotherapy in mid-2017. Further studies and presentations at ASCO will certainly add to this description, but are unlikely to change the basic scenario. Immuno-oncology now rules oncology, and IO must now catch up to itself with intensified mechanistic and clinical research in a grand collaboration of academic and industry science.
