Building A Universal AAV For Cancer

By Tyler Menichiello, Chief Editor, Bioprocess Online
Adeno-associated viruses (AAVs) are to gene therapy what smiling delivery trucks are to Amazon — i.e., they’re the reliable standard for therapeutic delivery. And just like Amazon, a company that used to exclusively deliver books, has moved into the business of delivering anything you can imagine (from furniture to groceries and electronics) so too are AAVs being adapted for broader use beyond monogenic disorders — particularly, in cancer.
One company is taking this a step further. Siren Biotechnology is working to create a universal AAV immuno-gene therapy that, much like the name implies, can be used “universally” to treat a variety of solid cancers. Unlike traditional gene therapies that deliver functional copies of a gene to treat monogenic diseases, Siren’s immuno-gene therapy delivers genes that code for cytokines to trigger an anti-tumor immune response.

Why Use Cytokines As A Payload?
In identifying the biggest challenges facing AAV gene therapies, Paulk says her lab kept coming back to one specifically: “Every AAV therapy on the planet is bespoke for a single indication — they’re one for one.” Because AAV gene therapies are usually developed for specific and unrelated rare diseases, it’s difficult to build on top of existing disease programs. “You very often don’t get to leverage learnings from your first program into the second program because hardly any of the component parts are shared,” Paulk explains. “By the time you start your second program, there’s a new best promoter, a new capsid, a new payload, a new way to manufacture and purify your virus — there’s all these new things.”
“We wanted to kind of take a step back and ask a really audacious question, which was: ‘Could you make a universal AAV gene therapy where none of the components ever changed, including the payload?’” Such an AAV would require a heavy lift in early development but make subsequent indications and clinical research much easier and cheaper, according to Paulk.
Paulk’s team at UCSF began thinking about what kind of payloads could have a broad therapeutic effect — broader than rare Mendelian genetic diseases where a single gene is missing. What kind of payloads can be put inside a virus? What payloads can you deliver that would do something of interest therapeutically? What could modulate cellular behaviors, interactions, signaling, and states?
“We took a kind of bioinformatic approach to think through what potential payloads could do all these things,” Paulk tells me. The list grew as her team came up with various ideas: transcription factors, cytokines, chaperones, factors that modulate protein degradation and cellular adhesion. Rather than testing one or two, Paulk says, her team made libraries of these potential gene therapies, “and one of the libraries we made was an engineered cytokine library.”
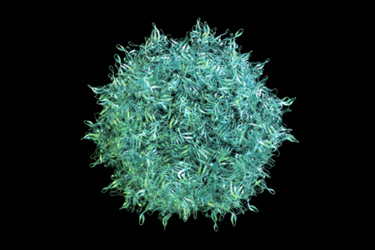
Cytokines are a diverse category of signaling proteins that regulate and modulate the immune system, and they’re involved in everything from allergic reactions to fighting infections and surveilling the body for cancer. “We were excited about cytokines simply because they’re these very pleotropic things that your body makes.”
“We weren’t necessarily focused on making the world’s first universal gene therapy for oncology,” Paulk says, “but we were excited about this very multi-acting library of payloads that we’d developed, because they might be universal in being able to treat many, many things.” One of the first use cases her team began testing cytokines in was oncology, “which was a bit heretical for an AAV company.”
How Siren Universalized An AAV
AAVs are not oncolytic viruses — i.e., viruses that target and kill cancer cells. “There had never been an AAV in oncology before, and so we got excited about just testing these as a use case,” Paulk says. This testing ultimately turned into Siren’s lead technology platform, its universal immuno-gene therapy.
So, how do you actually universalize an AAV? The key, Paulk says, is local delivery — and having a payload that doesn’t change with each new indication.
“All the tropisms and serotypes are still at play when you’re administering these things systemically,” she explains. “But you can kind of bypass all of that if you’re delivering it directly to a tumor.” It’s not hard to get these “promiscuous” AAV capsids inside the cell once they’re “at the gate.”
“If you can get an AAV to the cell surface, it will almost certainly go in,” Paulk says. The capsid type doesn’t matter. “In our case, what makes it universal is more at the payload level. We’re not delivering a gene that you’re missing due to a monogenic disorder. We’re delivering a multi-acting, pleotropic cytokine.”
Deciding Initial Indications
Therapeutic benefits aside, the major advantage of Siren’s universal AAV immuno-gene therapy is the dramatically reduced cost of subsequent clinical trials after the first (assuming these trials are targeting multiple cancer types in the same tissue). “Your first trial will be just as expensive as every other AAV gene therapy trial,” Paulk explains. “But for your second program in that same tissue, because everything stays the same — the same GMP product, the same data safety package, the same manufacturing process — you get to leverage all your learnings from that first trial to make the second program much easier, cheaper, and faster.” By taking this approach, Paulk says, the company should be able to scale its program with each subsequent trial.
However, with a “universal” AAV treatment that can (hypothetically) treat most solid tumors, how does a company like Siren decide which cancer/indication to start with? That decision needs to be data-driven, according to Paulk. “It should not be, what is everyone else going after? What’s hot right now? What’s investible?” If we imagine this decision as a funnel, she says, “right at the outer edge of the funnel, at the widest point — that should be data-driven. Do you have data that suggests patients with a particular cancer type, subtype, or particular set of confounding factors might be responsive?”
Whatever data you have access to — whether it’s genomic data, epigenomic data, transcriptomic data, proteomic data — so long as it’s clinically relevant, should inform this first indication. “Then you go down one step of the funnel and think about well, what tissues should we go after?” Paulk continues. “So, you may have narrowed the list of cancers down to 1,000. Which of these possible cancers are in tissues that are currently accessible with the capsids we have access to and the delivery routes our clinical colleagues know how to use?”
Then, it’s a matter of continuing down the funnel and asking increasingly specific questions. “Which ones have markets large enough that are investible with venture capital dollars? Meaning, it can’t be a very rare cancer with 100 patients,” she says. “Are you only going into adults, or are you also going after pediatric indications? What’s the competitive landscape as far as other drugs and modalities?”
As you continue down the funnel, asking questions that are a mix between scientific and corporate strategy, the list gets smaller and smaller — into double digits. “Then, as a scientist, you go out and start testing it,” Paulk says. “You start testing it and looking to see where things show the most positive signal and use that as your north star.” In addition to testing, Paulk says, Siren relies on artificial intelligence to predict the most-promising indication. The company is collaborating with WhiteLab Genomics and utilizing its AI-powered platform to accelerate the identification of new indications.
